Dealing with heel fat pad syndrome can be tough – the fat pad above my heel isn't as cushioned as it should be. Thin padding leads to pain during daily activities like walking and standing. Factors like age, injuries, or tight footwear could exacerbate the discomfort. Physical therapy and cushioned shoe inserts are some remedies. Considering more prevention tips could be helpful. Learning about the condition and treatments might shed more light on ways to manage this syndrome.
Understanding Heel Fat Pad Syndrome

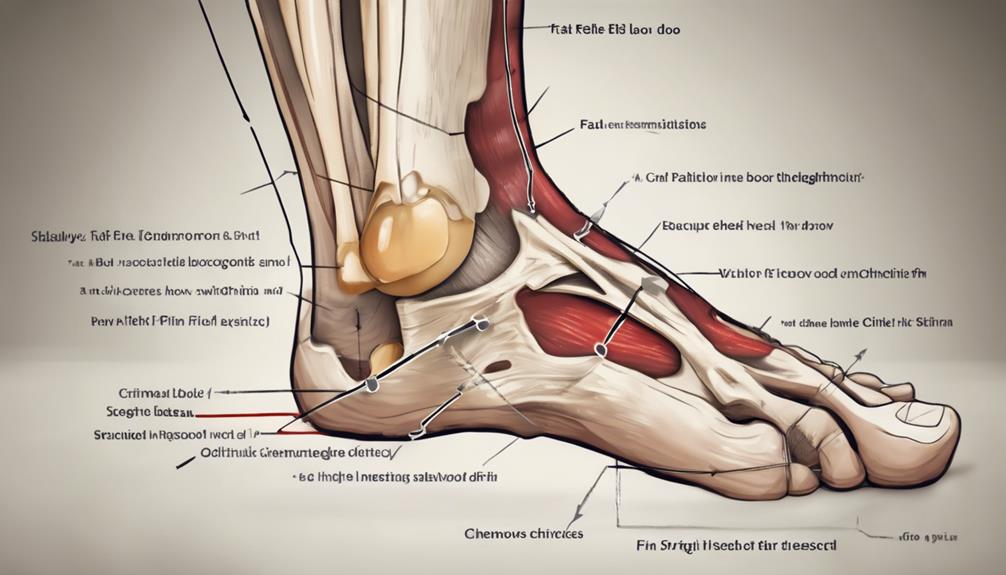
Heel Fat Pad Syndrome occurs due to thinning of the specialized adipose structure above the calcaneum and proximal plantar fascia. This thinning affects the heel fat pad's ability to cushion and support the foot adequately, leading to pain in the heel area, particularly when engaging in weight-bearing activities. The plantar fat pad, an essential component in shock absorption during walking and running, can undergo atrophy, further exacerbating the discomfort experienced.
Understanding the complexities of Heel Fat Pad Syndrome is essential in addressing the discomfort and limitations it brings. The plantar fat pad plays a crucial role in distributing pressure evenly across the foot, and any alterations to its structure can result in localized pain and reduced functionality. Heel fat pad syndrome challenges the foot's natural biomechanics, causing disruptions that manifest as discomfort and hindered mobility.
As individuals seeking innovation in foot health, it's important to comprehend the intricacies of this condition. By recognizing the impact of fat pad atrophy on heel health, we can explore creative solutions that go beyond conventional treatments. Embracing a deeper understanding of how the heel fat pad functions and its susceptibility to changes allows for the development of novel strategies to alleviate pain and enhance overall foot performance.
Risk Factors and Causes
Investigating the risk factors and causes of heel fat pad syndrome reveals a spectrum of influences on foot health and function. Age-related changes play a significant role, as the fat pad undergoes alterations in thickness and elasticity over time, making it more susceptible to damage. Trauma, such as injuries or surgeries in the foot area, can lead to fat pad atrophy, leaving delicate tissues exposed to strain and pressure. Additionally, obesity can exacerbate the condition by placing excessive stress on the heel fat pad during weight-bearing activities.
Engaging in repetitive high-impact activities is another common cause, as the continuous pounding on the heel can wear down the fat pad and contribute to discomfort. Women are particularly at risk due to the frequent use of high heels and tight footwear, which can compress and impact the heel fat pad negatively. Individuals with structural foot issues, family history of foot problems, arthritis, diabetes, or those taking certain medications are also more prone to developing heel fat pad syndrome due to the various underlying factors that affect foot health.
Signs and Symptoms

Upon experiencing Heel Fat Pad Syndrome, individuals typically notice deep, bruise-like pain in the middle of their heel. This discomfort can escalate with prolonged walking or standing, especially on hard surfaces. The pain may be more pronounced on one side of the heel, making each step a reminder of the underlying issue. As the symptoms progress, mobility can become compromised, impacting daily activities and overall function. The sensation of aching in the heel can disrupt one's quality of life, prompting a search for solutions to alleviate the persistent discomfort.
When faced with heel fat pad syndrome, the signs aren't merely physical but also emotional, as the frustration of limited movement sets in. The middle of the heel becomes a focal point of concern, triggering a cascade of challenges that extend beyond mere pain. The inability to engage fully in activities due to the nagging discomfort can be disheartening. Recognizing these signs and symptoms early on is important for prompt intervention and effective management. By addressing the manifestations of the syndrome proactively, individuals can regain control over their mobility and work towards restoring their heel health.
Diagnosis Methods
When diagnosing heel fat pad syndrome, healthcare providers commonly use imaging techniques like X-ray or ultrasound to assess fat pad thickness.
Clinical assessments, focusing on pain location and tenderness, play an important role in identifying this condition.
These methods are essential in distinguishing heel fat pad syndrome from other causes of heel pain.
Imaging for Diagnosis
I rely on imaging methods like X-ray, ultrasound, and MRI to diagnose heel fat pad syndrome. X-ray reveals fat pad atrophy or displacement in the heel, while ultrasound evaluates calcaneal fat pad thickness and elasticity. MRI provides detailed soft tissue images, essential for identifying fat pad abnormalities.
These imaging tools play an important role in confirming heel fat pad syndrome, aiding in making informed treatment decisions. By utilizing these innovative methods, we can accurately assess the condition of the fat pad and surrounding structures, leading to tailored treatment plans.
The precise visualization offered by X-ray, ultrasound, and MRI empowers clinicians to diagnose heel fat pad syndrome efficiently, ensuring appropriate interventions for patients.
Clinical Assessment Methods
Clinical assessment methods play a crucial role in diagnosing heel fat pad syndrome by evaluating symptoms such as deep heel pain and tenderness. During physical examinations, healthcare providers palpate the heel pad, assess for thickness changes, and observe gait patterns. Imaging tests like X-rays, ultrasounds, and MRIs help in diagnosing fat pad atrophy and evaluating tissue damage. Pressure testing with specialized devices can measure the cushioning capacity and elasticity of the heel fat pad. By combining symptom evaluation, physical exams, and imaging results, a thorough diagnosis of heel fat pad syndrome can be achieved.
| Clinical Assessment Methods | Description | Importance |
|---|---|---|
| Symptoms Evaluation | Assess deep heel pain and tenderness | Key in identifying the presence of heel fat pad syndrome |
| Physical Examination | Palpate heel pad, check thickness, observe gait | Provides insights into tissue damage and gait abnormalities |
| Imaging Tests | X-rays, ultrasounds, MRIs for diagnosis | Helps visualize fat pad atrophy and tissue damage |
Treatment Options

Conservative treatments for heel fat pad syndrome typically involve rest, ice, orthopedic footwear, and cushioned inserts to alleviate pain and reduce inflammation. When these methods aren't sufficient, there are innovative treatment options available to address heel fat pad syndrome effectively:
- Physical Therapy Interventions: Incorporating manual therapy techniques, specific exercises targeting the foot and ankle muscles, and utilizing low-dye taping can aid in restoring heel fat pad function and reducing discomfort.
- Orthotic Devices: Utilizing specialized orthotic devices such as heel cups and cushioned inserts can provide additional support and cushioning to protect the heel fat pad during weight-bearing activities, promoting healing and reducing pressure on the affected area.
- Advanced Interventions: For cases requiring more aggressive treatment, advanced options like injectable materials such as dermal fillers or autologous fat grafting can be considered to augment the heel fat pad and improve its shock-absorbing capabilities, ultimately enhancing overall function and comfort.
Prevention Strategies
Implementing appropriate preventive measures is vital in reducing the risk of developing heel fat pad syndrome and maintaining ideal foot health. To prevent heel pad syndrome, it's important to prioritize wearing proper footwear with dense cushioning and adequate support. Opting for athletic shoes during weight-bearing activities can help absorb impact and reduce strain on the heel pad. Avoiding high heels is also recommended as they can contribute to increased pressure on the heel, potentially leading to fat pad issues.
Additionally, it's advisable to limit the intensity and duration of weight-bearing activities to prevent overloading the heel pad. Refraining from walking barefoot on hard surfaces can also minimize the risk of developing heel fat pad syndrome. When selecting footwear, prioritize cushioning that provides adequate support and protection for the heel pad.
Staying informed about prevention techniques through articles, studies, and videos can further assist in maintaining foot health. Consistently following these preventive measures is key to significantly reducing the likelihood of experiencing heel fat pad syndrome and the associated discomfort. By being proactive and mindful of footwear choices and activities, individuals can safeguard their heel pads and promote overall foot well-being.
Conclusion
In the journey to address heel fat pad syndrome, we've explored the hidden depths of this condition and investigated various solutions.
Like a diver exploring the ocean depths, we've delved into the causes, symptoms, and treatment options with a sense of curiosity and determination.
By exploring these waters, we can find relief and take steps towards healing our heels.
Just as the tide ebbs and flows, we can rise above this challenge and walk with comfort once again.